Mens Health
Performed by Dr. David Wetherell
Men's health conditions can affect fertility, sexual function, comfort, and quality of life. This page outlines common male health procedures performed by Dr David Wetherell, with clear information about what each procedure involves, when it may be recommended, and what to expect before and after treatment.
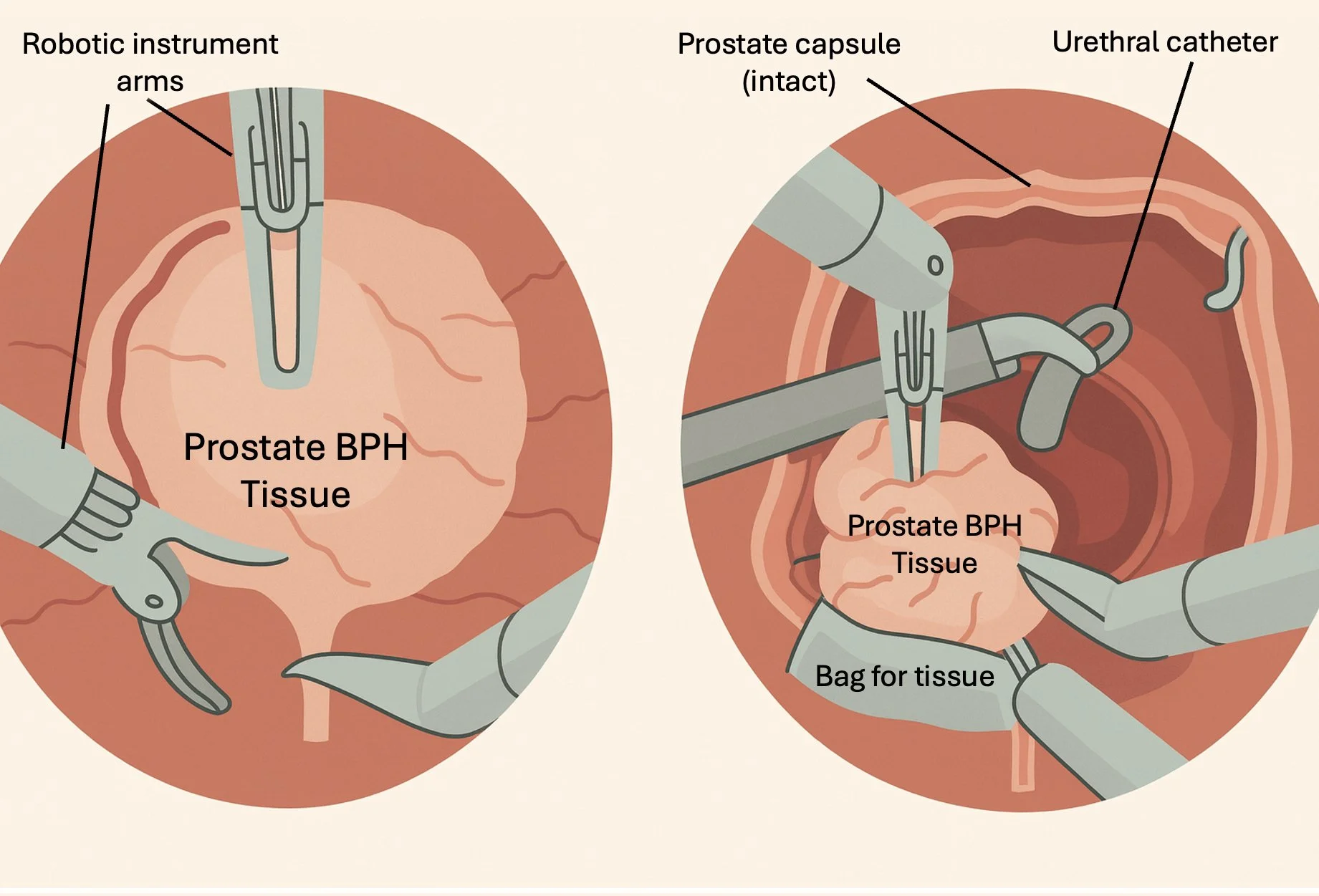
Robotic Simple Prostatectomy
•
Robotic or Laparoscopic Nephrectomy
•
Robotic or Laparoscopic Partial Nephrectomy
•
Robotic or Laparoscopic Nephro-Ureterectomy
•
Robotic or Laparoscopic Pyeloplasty
•
Retzius-Sparing Robotic Radical Prostatectomy
Robotic Simple Prostatectomy • Robotic or Laparoscopic Nephrectomy • Robotic or Laparoscopic Partial Nephrectomy • Robotic or Laparoscopic Nephro-Ureterectomy • Robotic or Laparoscopic Pyeloplasty • Retzius-Sparing Robotic Radical Prostatectomy
Vasectomy
The Key Things to Know:
A vasectomy is a simple and reliable form of permanent male contraception. It involves dividing and sealing the vas deferens (the tubes that carry sperm from the testicles) to prevent sperm from entering the semen.
What It Is
The procedure is typically performed under local anaesthetic in a clinic or general anaesthetic in a day surgery setting. A small puncture or incision is made in the scrotum to access the vas deferens on each side. The tubes are then divided, sealed, and the small wound closed - often without stitches. The testicles continue to produce sperm, but it is absorbed naturally by the body.
When It's Needed
A vasectomy is suitable for men who: - Have completed their families or do not wish to have children - Seek a permanent and highly effective contraceptive method - Understand that reversalprocedures are not always successful
Surgery Diagram
Benefits
Permanent and highly effective contraception (>99% success rate)
Simple, quick, and low-risk procedure
No ongoing contraception required for partner
Does not affect testosterone, libido, or erections
Risks
Mild bruising, swelling, or discomfort
Infection or bleeding under the skin (haematoma)
Rare chronic scrotal pain (post-vasectomy pain syndrome)
Small chance of vas deferens reconnection (failure rate <1%)
What to Expect After Surgery
You can usually go home shortly after the procedure. Mild discomfort is common for a few days. Supportive underwear, rest, and ice packs can help reduce swelling. You must continue using alternative contraception until semen analysis confirms no sperm - usually after 12 weeks or 20 ejaculations.
FAQs
-
No - testosterone levels, erections, and libido remain normal.
-
Light duties after 1-2 days; avoid heavy exercise for a week.
-
Reversal surgery is possible but not always successful, so it should be considered permanent.
Hydrocele Surgery (Hydrocelectomy)
The Key Things to Know:
Hydrocele surgery, or hydrocelectomy, is performed to remove a fluid-filled sac (hydrocele) surrounding the testicle. The condition is benign but can cause scrotal swelling, discomfort, or cosmetic concern.
What It Is
Under anaesthesia, a small incision is made in the scrotum or groin. The fluid is drained, and the sac lining is either removed or stitched (plicated) to prevent recurrence. The operation usually takes 30-45 minutes and is a day procedure.
When It's Needed
Hydrocele surgery is recommended when:
The swelling is large, tense, or uncomfortable
There is recurrent fluid accumulation - Infection, hernia, or tumour needs to be excluded
The appearance causes distress or inconvenience
Surgery Diagram
Benefits
Simple and effective correction of swelling
Day surgery with short recovery time
Excellent cosmetic and functional outcome
Risks
Bruising and swelling of the scrotum
Temporary discomfort or tightness
Infection or haematoma (blood collection)
Rare recurrence of hydrocele
Rare injury to the testis or surrounding structures
What to Expect After Surgery
Most patients go home the same day. Some swelling or bruising is expected for 1-2 weeks. Supportive underwear, rest, and ice packs can help reduce discomfort. Avoid strenuous activity and sexual activity for about 2 weeks.
FAQs
-
No, hydrocele repair does not affect sperm production or testosterone.
-
Recurrence is uncommon but can happen in a small percentage of cases.
-
Yes, if both sides are affected, they can be treated during the same procedure.
Circumcision
The Key Things to Know:
Circumcision is a surgical procedure to remove the foreskin, the retractable fold of skin that covers the head of the penis. It is performed for medical, functional, or personal reasons. In adults, circumcision is usually recommended for tight foreskin (phimosis), recurrent infections, or pain.
What It Is
Circumcision involves removing the foreskin under local or general anaesthetic. The exposed skin edges are closed with dissolvable stitches. The operation typically takes 20-40 minutes and is done as a day procedure. The goal is to relieve tightness and improve hygiene.
When It's Needed
Circumcision may be advised when:
The foreskin cannot be retracted (phimosis)
There are recurrent foreskin infections (balanitis)
There is pain during intercourse or hygiene difficulty
For cultural or religious reasons
Surgery Diagram
Benefits
Permanent solution for foreskin problems
Improved hygiene and reduced infection risk
Quick recovery and minimal discomfort
Usually day surgery
Risks
Mild pain, swelling, or bruising
Minor bleeding or infection
Rare scarring or over/under-removal of foreskin
Very rarely, narrowing of the urine opening (meatal stenosis)
What to Expect After Surgery
Most men go home the same day. Mild swelling and discomfort are normal for a few days. Keep the area clean and dry. Avoid sexual activity for 4-6 weeks and strenuous exercise for 2 weeks. Stitches dissolve naturally within 2-3 weeks.
FAQs
-
Local or general anaesthesia makes it comfortable. Mild soreness afterwards is common and managed with pain relief.
-
Most heal in 2-3 weeks, though swelling may take a little longer.
-
No - sensitivity and sexual performance remain normal.
Surgical Correction of Peyronie’s Disease
The Key Things to Know:
Surgery for Peyronie’s disease is performed when penile curvature or deformity interferes with sexual function. It aims to straighten the penis while preserving length, sensation, and erectile function. The operation is only done once the condition has stabilised for at least 6-12 months.
What It Is
Depending on the curvature and erectile function, there are three main types of surgery:
Plication surgery:
The longer side of the penis is shortened to straighten the curve (used for mild to moderate deformity).
Plaque incision/excision with grafting:
The plaque is cut or removed, and a graft is placed to restore length (used for severe curvature).
Penile prosthesis:
Used when erectile dysfunction is also present. Surgery is performed under general or spinal anaesthetic, usually as an overnight or short-stay procedure.
When It's Needed
Surgery may be recommended when:
The curvature is stable for at least 6-12 months
The penis bends enough to make intercourse difficult or painful
Non-surgical treatments have not provided improvement
Surgery Diagram
Benefits
Straightens the penis and restores function
High satisfaction rate when expectations are realistic
Can treat erectile dysfunction at the same time if required
Risks
Bruising and swelling for several days
Some loss of penile length (especially after plication)
Recurrence of curvature (uncommon)
Decreased sensation or erectile change (rare)
Graft or wound complications (rare)
What to Expect After Surgery
You’ll stay in the hospital for about 2–4 days. A catheter and drain are used temporarily. Mild abdominal discomfort, fatigue, and bloating are common early on. Gradual mobilisation is encouraged. You’ll usually return to light activity in 2–3 weeks and full recovery by 4–6 weeks. Follow-up cystoscopies and imaging are essential to monitor for recurrence.
FAQs
-
Straightening may reduce length slightly, depending on the technique used.
-
Recurrence is uncommon but can occur in severe or complex cases.
-
Usually after 6 weeks, once swelling and tenderness have settled.
Surgical Treatment for Varicocele
The Key Things to Know:
A varicocele is an enlargement of the veins that drain the testicle, similar to varicose veins in the legs. It can cause discomfort, testicular shrinkage, or fertility issues. Surgery, called varicocelectomy, repairs these veins to restore normal blood flow.
What It Is
Varicocele repair can be performed using several techniques:
Microsurgical varicocelectomy:
The most precise and effective method using a small incision in the groin and a microscope to tie off abnormal veins.
Laparoscopic varicocelectomy:
A keyhole approach that can treat both sides.
Radiological embolisation:
A non-surgical option where coils or plugs are inserted via a vein under imaging guidance. The procedure is usually done under general or local anaesthetic as a day case.
When It's Needed
Surgery may be advised when:
The varicocele causes discomfort or scrotal heaviness
Sperm quality is reduced on semen analysis
Testicular size is affected - Fertility treatment is being planned
Surgery Diagram
Benefits
Can improve sperm count and motility
Relieves discomfort and scrotal heaviness
Simple day surgery with a quick recovery
Risks
Mild pain or bruising for a few days
Hydrocele (fluid collection) in a small percentage of cases
Recurrence of varicocele (<5% with microsurgery)
Rare infection or bleeding
What to Expect After Surgery
You can go home the same day. Mild discomfort and swelling may occur and usually resolve within a few days. Wearing supportive underwear can help. Avoid strenuous exercise and sexual activity for about 2 weeks. A follow-up review or semen test may be arranged after 3 months if done for fertility reasons.
FAQs
-
Many men notice better sperm quality within a few months.
-
Yes - both sides can be repaired during the same operation.
-
Rare, especially with microsurgical techniques.
Orchidectomy (Removal of Testis)
What It Is
The operation is performed under general anaesthetic. A small incision is made in the groin (inguinal approach), and the affected testis is removed along with its spermatic cord. The tissue is sent for detailed pathology testing to determine cancer type and stage. The other testis remains and usually continues to produce testosterone and sperm.
The Key Things To Know
An orchidectomy (also called orchiectomy) is the surgical removal of one or both testicles. It is most commonly performed to treat testicular cancer, but may also be done for severe injury, infection, or hormone-related conditions. When done for cancer, it provides both diagnosis and curative treatment in many cases.
When It’s Needed
Orchidectomy is recommended when: - A testicular lump or tumour is detected on ultrasound and tumour markers are raised - There is confirmed or suspected testicular cancer - Severe infection, torsion, or injury has caused irreversible damage - In rare cases, for hormonal control of advanced prostate cancer
Surgery Diagram
Benefits
Provides definitive diagnosis and primary treatment for testicular cancer
Usually curative for localised tumours (>95% survival when detected early)
Short, low-risk day procedure
Minimal impact on sexual function when one testis remains
Risks
• Mild groin or scrotal discomfort for a few days
• Temporary swelling or bruising
• Infection (≈3%) or bleeding (≈2-3%)
• Psychological impact due to loss of a testis
• Rare chronic groin pain (<2%)
What to Expect After Surgery
You can usually go home the same day. Mild discomfort and bruising are common for several days. Most men return to light activity within a week. Stitches dissolve naturally. You’ll receive pathology results in about 1 week. Further treatment (such as chemotherapy or radiotherapy) may be needed if cancer is confirmed.
FAQs
-
Yes - the remaining testis usually maintains normal hormone production.
-
Yes, a silicone prosthesis can be inserted at the time of surgery or later if desired.
-
Usually not if the remaining testis is healthy, though sperm banking is recommended before cancer treatment.
Discover Expert Urological Care
I specialise in precision urology using the latest robotic and minimally invasive techniques. Explore my approach, my procedures, and the care I provide at every stage of your journey.